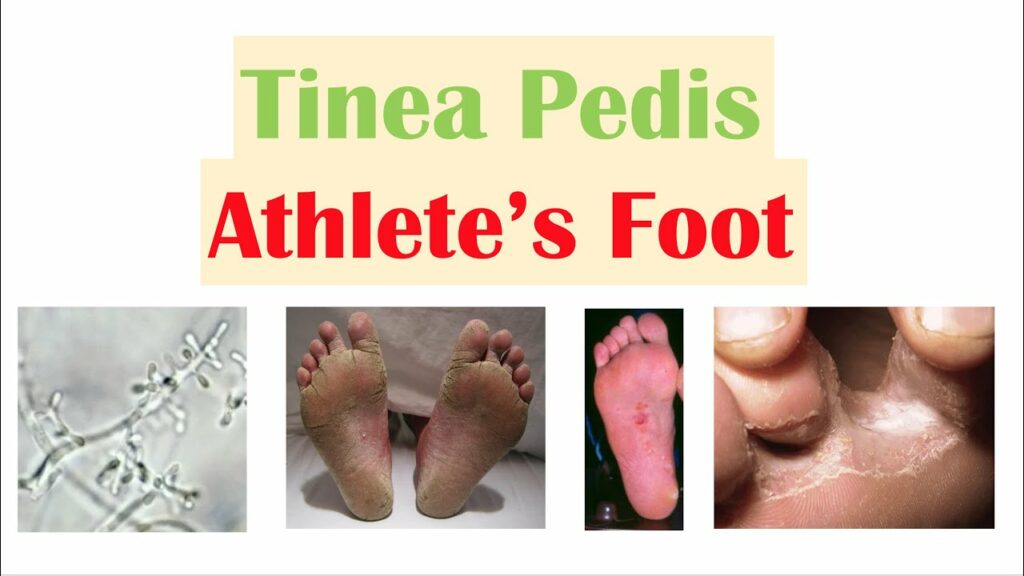
What is Athlete’s Foot?
Athlete’s foot, also referred to as Tinea Pedis, is a skin disease caused by a fungus, usually occurring between the toes, but it can also affect other areas of the feet. The fungus associated with athletes foot most commonly attacks the feet because shoes create a warm, dark, and moist environment that encourages fungus growth. Not all fungal conditions are athlete’s foot. Other conditions, such as eczema and psoriasis, may mimic athlete’s foot and can be difficult to distinguish to the untrainted eye.
How did I get Athlete’s Foot?
The warmth and dampness of areas around swimming pools, showers, and locker rooms are also breeding grounds for fungi. Because the infection was common among athletes who used these facilities frequently, the term “athlete’s foot” became popular.
Symptoms
The signs of athlete’s foot, singly or combined, include the following:
- Dry-looking skin
- Itching and burning between the toes, which may increase as the infection spreads to other parts of the feet
- Scaling or peeling skin
- Inflammation or swelling
- Blisters, which often lead to cracking or peeling skin to the feet and toes. When blisters break, small raw areas of tissue are exposed, which may cause swelling.
Athlete’s foot may spread to the soles of the feet and to the toenails. It can be spread to other parts of the body by those who scratch the infection and then touch themselves elsewhere. The organisms causing athlete’s foot may persist for long periods.
Home Care
It is important to keep the feet dry by using foot powder in shoes and socks. The feet should be bathed frequently and all areas around the toes dried thoroughly. If someone in your family develops athlete’s foot, disinfect home showers and tubs after each use to discourage transmission of infection.
When to Visit a Podiatrist
If you believe that you have a fungus infection that does not respond to proper foot hygiene and there is no improvement within two weeks, you should call our office.
Diagnosis and Treatment
Your podiatrist will determine if a fungus is the cause of the problem. If it is, a specific treatment plan, including the prescription of antifungal medication, applied topically or taken by mouth, may usually be suggested. Such a treatment appears to provide better resolution of the problem when the patient follows the course of treatment prescribed by the podiatrist; if it’s shortened, failure of the treatment is common.
Topical or oral antifungal drugs are often prescribed. If the infection is caused by bacteria and not fungus, antibiotics that are effective against a broad spectrum of bacteria, such as penicillin, may be prescribed.
It is important to continue to keep the feet dry by using recommended or prescribed foot powder in shoes and socks. The feet should be bathed frequently and all areas around the toes dried thoroughly. If someone in your family develops athlete’s foot, disinfect home showers and tubs after each use to discourage transmission of infection.
Prevention
It is easy to prevent athlete’s foot where bare feet come in contact with the fungus by practicing good foot hygiene. You can prevent fungal infection by practicing the following:
- Wash feet daily with soap and water; dry carefully, especially between the toes
- Avoid walking barefoot; use shower shoes in public showers.
- Reduce perspiration by using talcum powder
- Wear light and airy shoes
- Change shoes and socks regularly to decrease moisture
- Wear synthetic blend socks that wick away moisture, and change them frequently if you perspire heavily
